If you suffer from arthritis, you may have heard of both rheumatoid arthritis (RA) and osteoarthritis (OA). The word arthritis is confusing. It simply means 'swollen joint', the symptom that links these two conditions.
But what is the difference between them? And how can you tell if you have one or the other? In this blog post, we’ll look at the similarities and differences between RA and OA.
What is Rheumatoid Arthritis?
Rheumatoid Arthritis is an autoimmune disease where the body’s natural defense system attacks its own joints. It usually affects multiple joints, making it difficult for people with RA to carry out everyday activities. The main symptoms of RA include pain, swelling, stiffness, and joint deformity. People with RA often experience fatigue and a general feeling of being unwell.
The exact cause of RA is unknown; however, genetics, hormones and environmental factors are believed to play a role.
What is Osteoarthritis?
Osteoarthritis is a type of degenerative joint disorder that can affect any joint in the body. It causes a gradual breakdown of cartilage that cushions the joints and leads to pain, swelling, stiffness, and decreased range of motion in the affected area. OA typically occurs in older adults but can also be caused by prior joint injury or overuse.
Similarities between RA & OA
Both RA and OA are types of chronic inflammatory arthritis that cause joint pain, stiffness, swelling, and limited range of motion.
They can both be managed with medications such as non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroids.
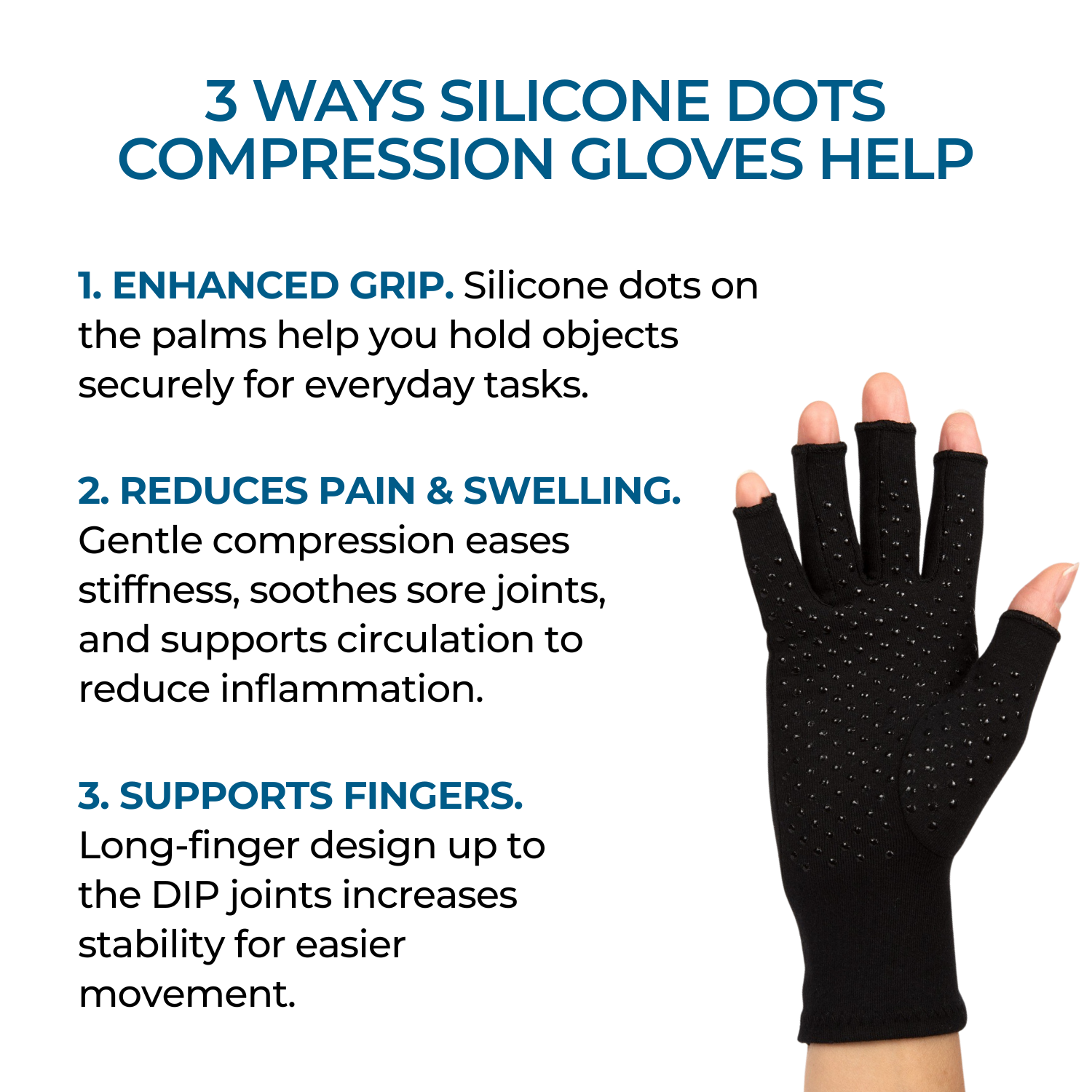
Other treatments such as physical therapy or lifestyle modifications may also help reduce symptoms associated with both forms of arthritis. Both conditions benefit from the use of adaptive aids like walking sticks, wrist braces and compression gloves.
What are the differences between RA & OA?
The main differences between RA and OA are their causes and severity levels. While OA is caused by wear-and-tear on joints due to age or injury, RA is caused by a malfunctioning immune system attacking healthy tissue in the body’s joints.
Additionally, while OA tends to affect one specific joint at a time (often older adults like knees), RA can affect multiple joints at once (typically younger adults like hands). RA can also affect other tissues in the body, including the eyes, lungs and heart.
Finally, OA tends to be less severe than RA; although it can still cause pain and disability over time if left untreated.
Diagnosis: How are OA and RA diagnosed?
When it comes to diagnosing rheumatoid arthritis (RA) and osteoarthritis (OA), the process typically begins with a physical exam. During this examination, your doctor will look for signs of swelling, redness or warmth in the affected joint(s). They may also ask about any symptoms you’ve been experiencing such as pain or stiffness.
Additionally, your doctor may perform imaging tests like X-rays or ultrasounds to get a better understanding of what is happening inside the joint. Blood tests are also commonly used to diagnose RA but not OA. The results from these tests can help rule out other conditions as well as provide information on how severe the condition is so that an appropriate treatment plan can be created.
Treatment: What are the treatments available for each condition?
When it comes to treating rheumatoid arthritis (RA) and osteoarthritis (OA), there are many options available.
For RA, treatment typically involves medications such as Non-steroidal anti-inflammatory drugs (NSAIDs), disease modifying drugs and biologics. In addition, lifestyle changes like exercise programs or diet modifications may also be recommended to help manage symptoms. Surgery is an option for severe cases of RA but is usually avoided if possible due to the risks associated with it.
For OA, treatments tend to focus on managing pain and preventing further damage from occurring. Common medications used include NSAIDS, corticosteroids injections into joints for short term relief as well as physical therapy exercises that can help improve flexibility and range of motion in affected joints.
Additionally, some people opt for joint replacement surgery if other treatments have been unsuccessful in relieving the pain or disability caused by the condition.
Prognosis: What is the outlook for each condition?
The prognosis for rheumatoid arthritis (RA) depends on the severity of the disease and how quickly it is treated. With early diagnosis and aggressive treatment, people with RA can often lead normal lives free from pain or disability. However, if left untreated or not managed properly, RA can cause long-term joint damage that may be difficult to manage. Additionally, RA increases your risks of other health complications such as cardiovascular disease so it’s important to stay on top of regular checkups with your doctor.
For osteoarthritis (OA), the outlook is generally more positive since OA cannot be cured but instead managed through lifestyle changes and medication aimed at reducing pain and inflammation in affected joints. Early intervention is key in preventing further deterioration of joints over time which can help improve mobility and quality of life for those with OA. Surgery may also be recommended if conservative treatments are unsuccessful in relieving symptoms; however this option should only be considered after discussing all potential risks involved first with a qualified healthcare professional.
Prevention: Can either of these conditions be prevented?
When it comes to preventing rheumatoid arthritis (RA) and osteoarthritis (OA), there are certain things you can do to reduce your risk. For RA, the exact cause is still unknown so prevention isn't always possible. However, research suggests that maintaining a healthy lifestyle may help lower your chances of developing RA as well as other autoimmune diseases. Eating a balanced diet rich in fruits and vegetables, getting regular exercise and avoiding smoking can all contribute to overall health which may in turn help prevent the onset of RA.
For OA, the best way to avoid it is by keeping joints strong and flexible with regular physical activity such as walking or swimming. Maintaining good posture when sitting or standing for long periods of time can also be beneficial in reducing strain on your joints over time. Additionally, if you suffer from an injury like sprains or strains make sure to rest until completely healed before resuming any activities again; this will decrease the chance of further damage occurring down the line.
Conclusion:
So there you have it – now you know how rheumatoid arthritis differs from osteoarthritis!
It's important to be aware of the differences between rheumatoid arthritis and osteoarthritis, as well as their symptoms, causes, diagnosis, treatments and prognosis.
Even though both conditions can worsen over time, there are ways to reduce the severity of both such as maintaining a healthy lifestyle and avoiding activities that could cause injury.
Both conditions can cause pain and disability if left untreated – so if you think you may be suffering from either condition it’s important to seek medical advice as soon as possible so that appropriate treatment options can be discussed with your doctor or healthcare provider.

































































Share and get 15% off!
Simply share this product on one of the following social networks and you will unlock 15% off!